4 days of chest pain
Responding to back up an Intermediate EMS unit. Found 64 year old male patient in back of EMS unit. Patient was alert and oriented stating he has had chest pain for the last 4 days. Pain comes and goes and he states the pain in his chest worsens when he moves. He also gets very short of breath with the least bit of exertion. When asked to describe his pain says, “It feels like a burning sensation along with heavy pressure, like someone is standing on my chest!” Pain is 8/10 and feels just like the previous MI he had back in the late 90’s. He has taken his nitro occasionally but it has not helped.
The patient is calm, skin is warm and dry but pale.
V/S are as follows:
BP: 114/60
Respiration: 16

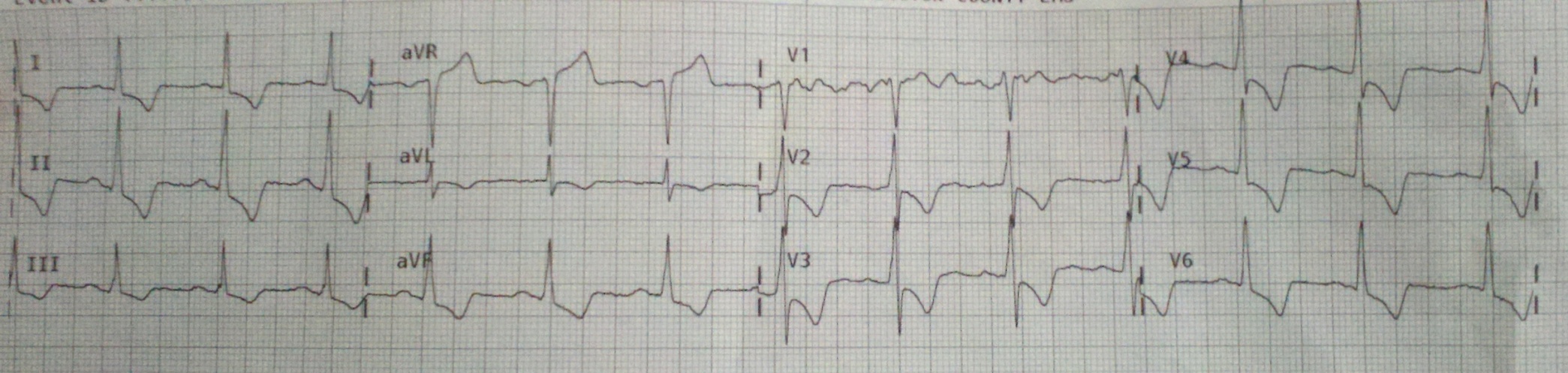


Neat posterior look! Looks STEMI to me.
This illustrates the difficulties and potential pitfalls of modified chest leads. What is abnormal? Are pathological Q-wave enough? With QRS complexes about 5 mm (small) even the slightest wandering baseline confounds the interpretation although the first complex in lead V9 appears to show 0.5 mm of J-point elevation. We need more practical experience with these leads to help interpret the results. Will be interested in finding out whether or not this was a left main, proximal LAD, 3-vessel disease, or some other cause of subendocardial ischemia. Either way, I think the patient has to be cathed. If you don’t cath and the patient codes that would be very bad. Very interesting 12-lead ECG!
@Tom, This EKG was transmitted to the receiving ER along with the modified leads as well. The receiving ER did not seem to be too concerned with this ecg or patient complaint. They placed this patient in a room on arrival. The receiving doctor came in and talked to the patient for a few minutes while the ecg tech ran another 12 lead, which showed exactly what the 12 lead that I sent showed. He stated the ecg was “Ugly” but did not know if it was new ugly or old ugly and would have to take a look at an old ecg. He walked over to the computer and pulled up an ecg or the patient. That ecg, showed that this was all new. He immediately called a Code STEMI and the patient was taken to the cath lab. I am hoping to get feedback from this case as soon as it becomes available and post an update to this case. I too noticed that there was about 0.5mm ST elevation in lead V9 but given the small size of the qrs in lead V9 i considered 0.5mm to be significant.
great case. Only question is about transmitting the alternate leads as the ER can’t see what we re-labelled. Calling them to explain would probably just confuse them… eh?
@eff dogg personally I have not had any issues with sending modified 12 leads then notifying the ER of the change
at least the receiving doc was aware enough to be paying attention
i agree with “burned-out medic”! the doc was at least paying attention and didn’t dismiss the patient.
@Tom I agree. I’m not sure that this counts as a STEMI. V8 and V9 are a long way around – I would hazard a guess that they are simply seeing the reciprocal of V1 and V2. In fact if you mentally flip V8 over it looks just like V1 and V9 flipped is pretty close to V2. They are proportionally smaller than V1 and V2 as they are farther away from the depolarising muscle (measured voltage drops off with distance – http://bit.ly/hKLhlO). Other modified leads like V4R are probably more important because they examine parts of the heart missed by the standard leads. But V8 and V9 not sure….someone should study it! In any case, this looks a little left main-like (had he had previous CABG?). Off to the lab.
it could be pericarditis
subacut p.
Depression in all standard leads while there is elevation in aVR! It would be fine to see another EKG with a better tracing in V1 to see if there is elevation as well.
POSTERIOR WALL MYOCARDIAL INFARCTION
This is very unlikely to be posterior STEMI. It is most likely to be severe global subendocardial ischemia due to 3-vessel disease or critical left main ACS. This is because:
1. ST depression precordial: J point returns to near baseline, then downsloping
2. ST depression out to V6, not limited or even maximal in V1-V4
3. ST depression in limb leads diffusely
4. ST elevation in aVR (which must be there with all the diffuse limb lead STE
5. STE in leads V7-V9 can also be seen as reciprocal to ST depression in V2-V4
The patient would be best off going to the cath lab, but it may be controllable with medical therapy alone. Thrombolytics would be contraindicated.
Steve Smith of Dr. Smith’s ECG Blog
NSTEMI anterolateral
What was your Treatment for this Patient?
02, ASA, NTG, bilat IV’s transport to a PCI center that was 5 mins away